Happy National Aphasia Awareness Month to you all! In honor of National Aphasia Awareness Month, and in recognition of the upcoming, All About MossRehab Through the Arts, we are highlighting people with aphasia who are making a contribution to their communities through the arts.
Continue Readingaphasia
Aphasia and the Arts: Poetry
Happy National Aphasia Awareness Month to you all! In honor of National Aphasia Awareness Month, and in recognition of the upcoming, All About MossRehab Through the Arts, we are highlighting people with aphasia who are making a contribution to their communities through the arts.
Continue ReadingMusic and Aphasia
As we wind down our activities for National Aphasia Awareness Month, we’re so pleased to feature this guest post from our own, Roberta Brooks, CCC-SLP!
Continue ReadingJune is National Aphasia Awareness Month!
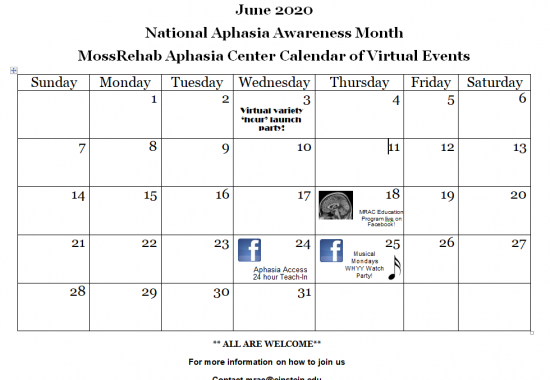
At the MossRehab Aphasia Center, every month is Aphasia Awareness Month, but we always plan special events for June. Please join us and help spread the word about aphasia!
Continue ReadingPersonalizing communication practice
For people with aphasia, having to stay at home can make it more difficult, but also more important, to keep practicing language and communication.
Continue ReadingStaying connected during COVID-19
We’ve all been affected by COVID. For people with aphasia, the quarantine can make social isolation even worse.
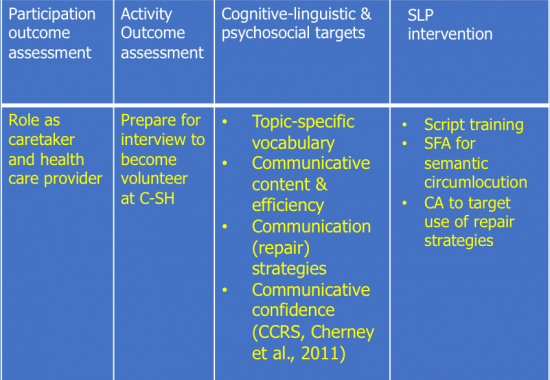
Continue ReadingOutcome Measurement based on the Life Participation Approach to Aphasia: Vol. 1
The MossRehab Aphasia Center was founded on the principles of the Life Participation Approach to Aphasia (LPAA, Chapey et al., 2000). These principles include:
Continue ReadingDr. Wlotko Receives NIH Grant for Study of Sentence Comprehension in Aphasia
MRRI Institute Scientist Edward Wlotko, PhD, will serve as principal investigator of a subcontract award totaling more than $1M from the National Institutes of Health. The research is part of a grant, entitled “Cognitive control and sentence processing in aphasia,” received by Malathi Thothathiri, Ph.D., of the Department of Speech, Language & Hearing Sciences at George Washington University. Dr. Thothathiri is a former postdoctoral fellow at MRRI. Continue Reading
Creating a Path to Improved Naming in People with Aphasia
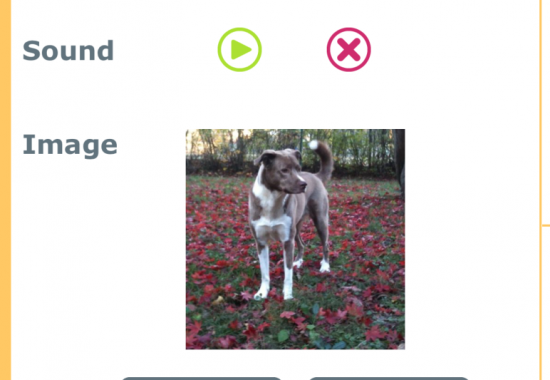
Aphasia can be quite frustrating for people who struggle to communicate. In addition to naming difficulties, some people with aphasia experience comprehension impairment, where hearing or reading the name of an object conveys the wrong image or meaning.
Erica Middleton, PhD, has been studying naming problems for eight years. Her last six years have been spent researching how people with aphasia can relearn and comprehend names, first as a Post-Doc at Moss Rehabilitation Research Institute (MRRI), and now as the Institute Scientist leading MRRI’s Language and Learning Laboratory.
In this video, Dr. Middleton talks about a five year, $2.4 million grant she received from the National Institutes of Health that will lead to a theory of learning needed to advance aphasia rehabilitation.
Myrna Schwartz Appears on Aphasia Access Podcast
Mryna Schwartz, PhD, co-founder of the Moss Rehabilitation Research Institute, recently discussed best practices in aphasia care as part of the Aphasia Access Conversations podcast series.
In a conversation with Janet Patterson, PhD, Dr. Schwartz discussed the role of ethics and institutional review in clinical research activities that involve people with aphasia.
Dr. Schwartz headed MRRI’s Language and Aphasia Laboratory for many years.