Damage to a brain structure called the cerebellum causes a movement disorder called Ataxia. Derived from the Greek word for “lack of order,” Ataxia is marked by poor movement coordination. Ataxic movements have a “drunken” appearance, with lateral veering and oscillations. Many neurologic conditions such as stroke, multiple sclerosis, traumatic brain injury, and a host of genetic conditions can cause damage to the cerebellum, and the individuals affected often have disabling Ataxias that impair their balance, walking, arm movements, and speech. According to the U.S. National Ataxia Foundation, 15,000 – 20,000 people are estimated to have autosomal dominant genetic Spinocerebellar Ataxias in the United States, and tens of thousands more are affected by recessive and sporadic genetic ataxias, as well as other conditions that cause cerebellar damage.
There are no medications to treat Ataxia, leaving rehabilitation therapies like physical, occupational, and speech-language therapies as the only option for symptom management. However, rehabilitation outcomes are mixed in this population, with many individuals not benefiting from current intervention techniques. One reason for this may be that, in addition to its role in movement control, the cerebellum is critical to an important mechanism for learning new movement patterns. Many rehabilitation interventions try to train the brain to move the body in different ways to help compensate for neurologic conditions, and often, these techniques leverage the learning mechanism that depends on the cerebellum.
Research by Amanda Therrien, PhD, Director of the Sensorimotor Learning Laboratory at MRRI, has investigated whether a new training technique using binary reinforcement could help people with Ataxia improve their movement control. Using a combination of virtual reality and motion capture technology, binary reinforcement training aims to leverage a brain mechanism for learning new movements that does not depend as heavily on the cerebellum. Prior work from Dr. Therrien, published in the journals Brain and The Cerebellum, established that individuals with Ataxia can use binary reinforcement training to learn to adjust their arm movements and that it can be leveraged to help improve arm movement control. These findings emphasize that binary reinforcement training warrants further research to determine whether it can be applied to improve rehabilitation therapy for Ataxia more broadly.
One question that came out of Dr. Therrien’s previous work is related to the finding that, while most individuals with Ataxia were able to learn with binary reinforcement, a small percentage of study participants did not benefit from the training. The difference in training outcomes across individuals could not be explained by the severity or type of Ataxia, suggesting that the root cause of this variability in outcomes was more complex. Understanding the causes of variability in outcomes across individuals would advance our understanding of which individuals are most likely to benefit from binary reinforcement training, allowing streamlined screening for clinical trials as well as informing future work investigating whether the training technique can be modified to improve outcomes in individuals who respond poorly to the current protocol.
This past year, Dr. Therrien’s research group published a new study in the journal The Cerebellum that tested whether the historically underappreciated role of the cerebellum in movement perception could explain differences in learning across individuals. Movement perception relies heavily on a sense called proprioception (also called kinesthesia), which is how your brain knows where your body is in space when vision is absent. It is thanks to proprioception that you still know where your feet are, even though you may not be looking at them while reading this article. Proprioception is important for binary reinforcement training because the technique reduces visual information about movement outcomes to reduce dependence on cerebellum-dependent learning. Although cerebellar damage doesn’t impair primary proprioception (people with Ataxia have a normal sense of where their body is in space when they are not moving or if they are passively moved by another person or a device), it can interfere with proprioception when moving voluntarily. The degree to which cerebellar damage can interfere with the perception of voluntary movement varies across individuals and, like the response to binary reinforcement training, is not easily explained by Ataxia type or severity.
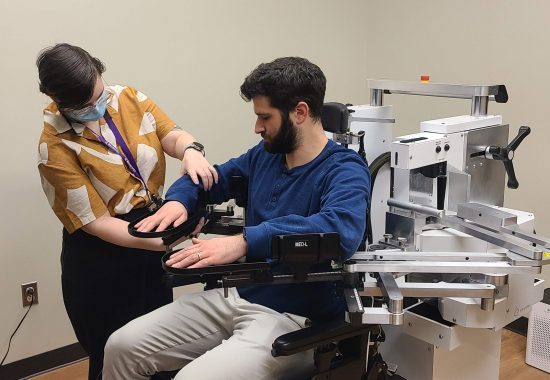
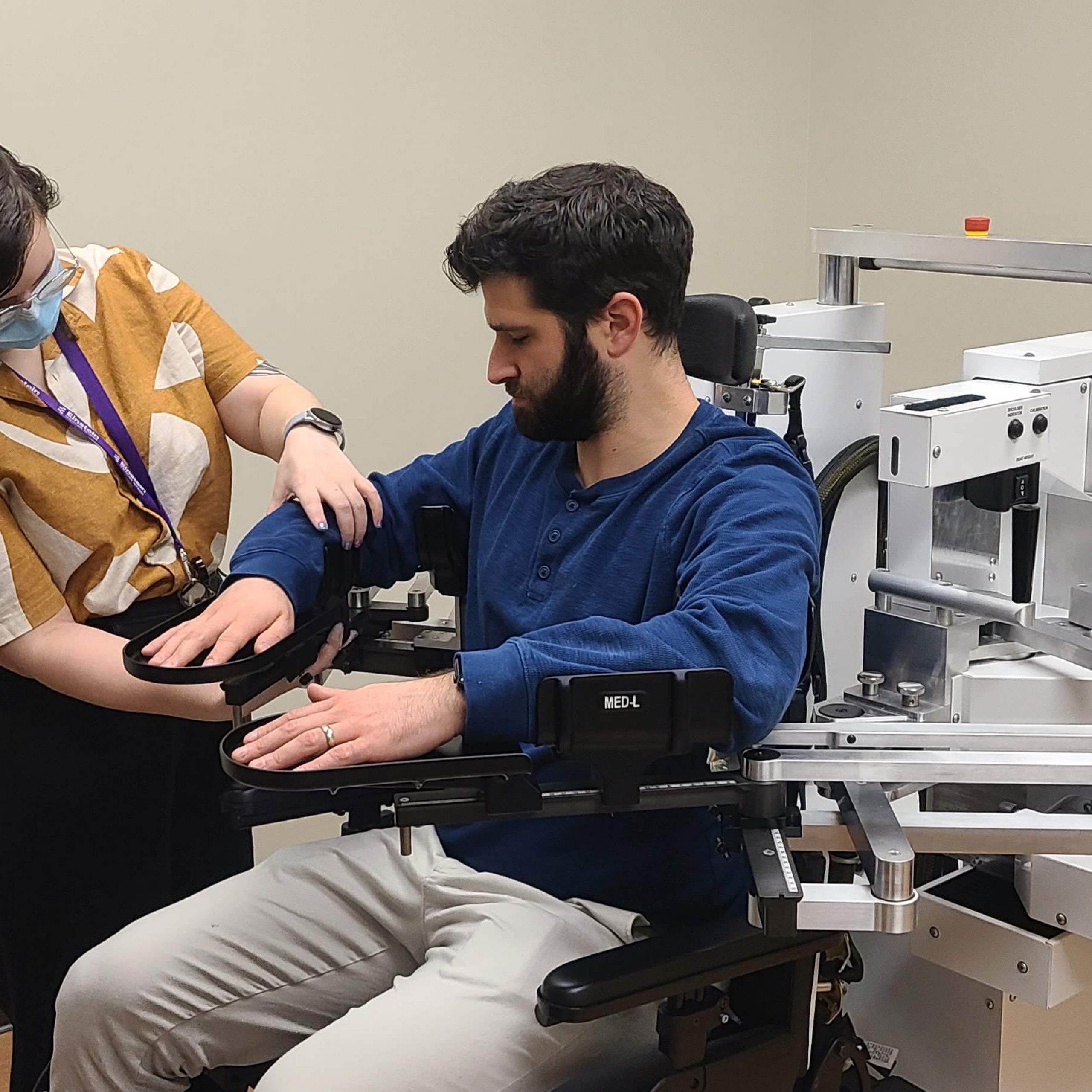
In Dr. Therrien’s recent study, a group of individuals with Ataxia performed a short binary reinforcement training task that required them to learn a new reaching movement. They then completed an assessment of their movement perception that tested the difference in proprioception between a condition in which they were passively moved by a robotic device and a condition in which they moved voluntarily. Dr. Therrien’s research group analyzed the relationship between the magnitude of learning achieved in the binary reinforcement task and performance in the movement perception assessment. The study team also included other variables in their analysis, such as the severity of participants’ arm movement impairment, their age, and their movement speed in the binary reinforcement task, to determine whether they also played a role in learning. The results showed a strong relationship in which a greater impairment in the perception of voluntary movement relative to the perception of passive movement was associated with a reduced response to binary reinforcement training. Replicating prior findings, none of the other variables tested exhibited relationships with the training outcome.
Overall, the findings suggest that tests of proprioception of voluntary movement may one day serve as a metric to predict which individuals with Ataxia might benefit from binary reinforcement training. This line of research in MRRI’s Sensorimotor Learning Laboratory is answering important questions that are critical for better understanding motor learning in order to develop more effective and more personalized treatments approaches for people with Ataxia.