Jane suffered a stroke that impacts the sensation, strength, and dexterity of one of her arms. She worked hard in inpatient neurorehabilitation, and assessments showed that her capacity to use the arm greatly improved. When she returned home, however, her spouse noticed that she continues not to use the affected arm much in daily activities, preferring to rely on the other arm or to ask others for help. In fact, over time her use of the affected arm actually seemed to be decreasing.
One of the most challenging aspects of neurorehabilitation of stroke is that many individuals with adequate sensory-motor recovery and capacity to use their impaired arm do not actually do so.
Instead, there is a maladaptive pattern of over-use of the relatively intact arm, resulting in a vicious cycle in which the affected arm loses the gains that resulted from neurorehabilitation. Can we identify the factors that make people likely to show this pattern of non-use?
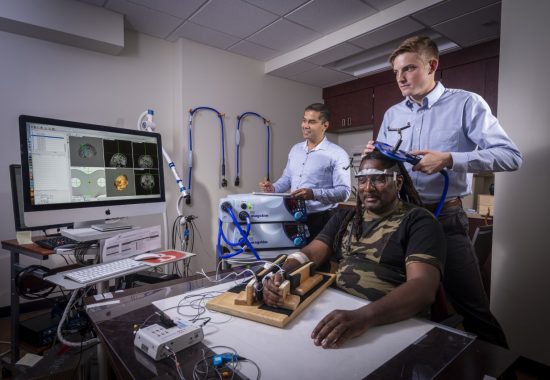
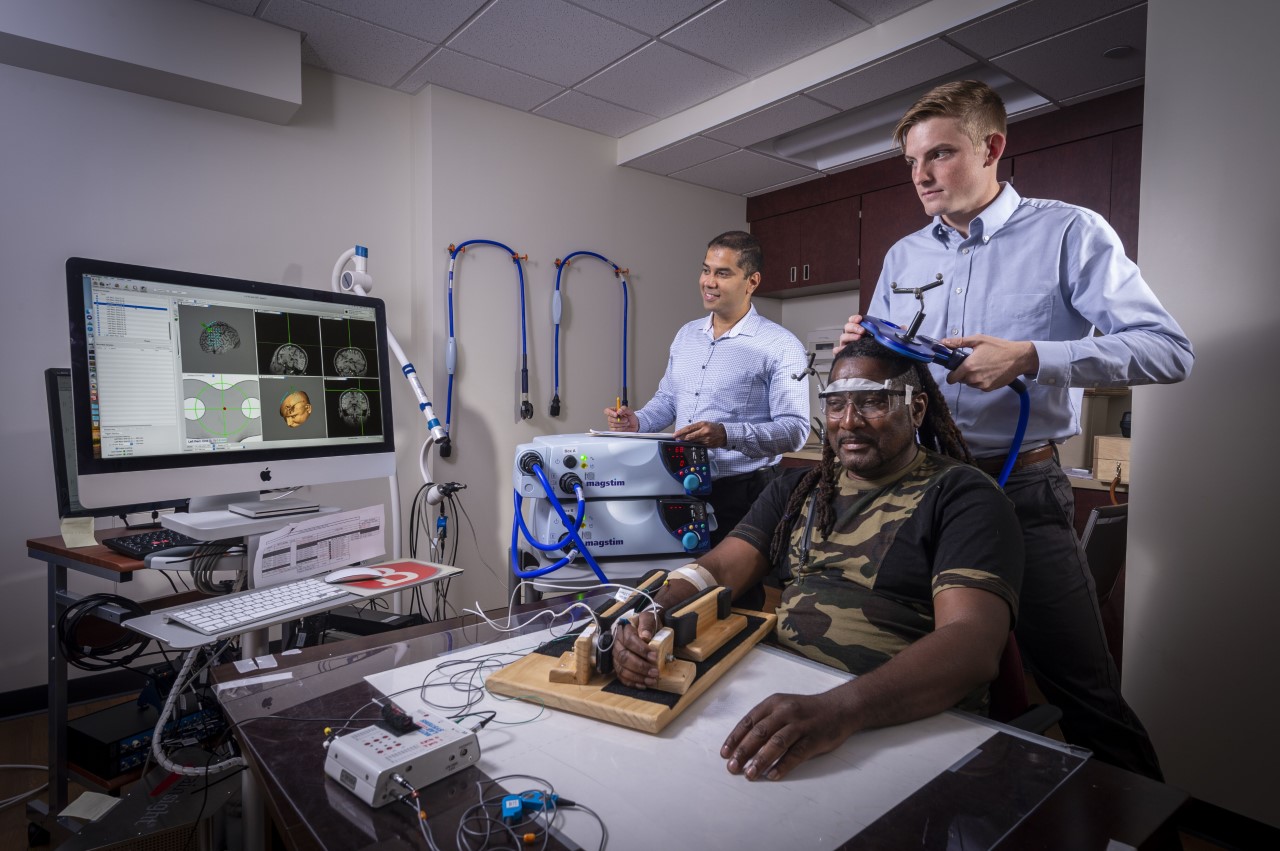
One obvious factor might be the ability level of the affected arm: people clearly favor their less-impaired arm if the impaired arm is particularly limited. Working with a team from University of Southern California (USC), the MRRI Cognition and Action Lab headed by MRRI Associate Director Laurel Buxbaum, PsyD, performed a study showing that even when the severity of arm impairment is taken into account, a second factor—sustained attention – plays an important role in determining whether individuals are likely to use that arm.
The researchers suggest that this pattern fits with the importance of sustained attention and ability to expend effort in a variety of cognitive and motor tasks, and with the idea that arm use occurs on the basis of an implicit cost-benefit analysis. In individuals who have suffered a stroke, the reduced sensory-motor capacity of the impaired arm requires extra sustained attention and effort to overcome. That is, movement comes at a greater “cost”. At the same time, however, the stroke diminishes the ability to deploy attention and effort. “To shift the cost-benefit relationship”, says Dr. Buxbaum, “we need to increase the degree to which use of the impaired arm is associated with reward”.
Neurorehabilitation programs can shift the cost-benefit relationship to favor arm use in a variety of ways. Some direct ways including “gamifying” arm use via virtual reality and other motivating games, or allowing accumulation of points or rewards for arm use. In addition, therapists can use goal-setting, peer support groups, family involvement with goals, and frequent check-ins to boost the reward associated with using the impaired limb. In fact, therapies that have been associated with such benefits (sometimes termed “transfer packages”) have generally been more successful than those that do not.
Dr. Buxbaum and her colleagues from USC recently published a peer-reviewed study on the factors determining non-use in the journal Neurorehabilitation and Neural Repair. Along with MRRI Institute Scientist Shailesh Kantak, PhD, the researchers are in the process of developing a funding proposal for follow-up research.