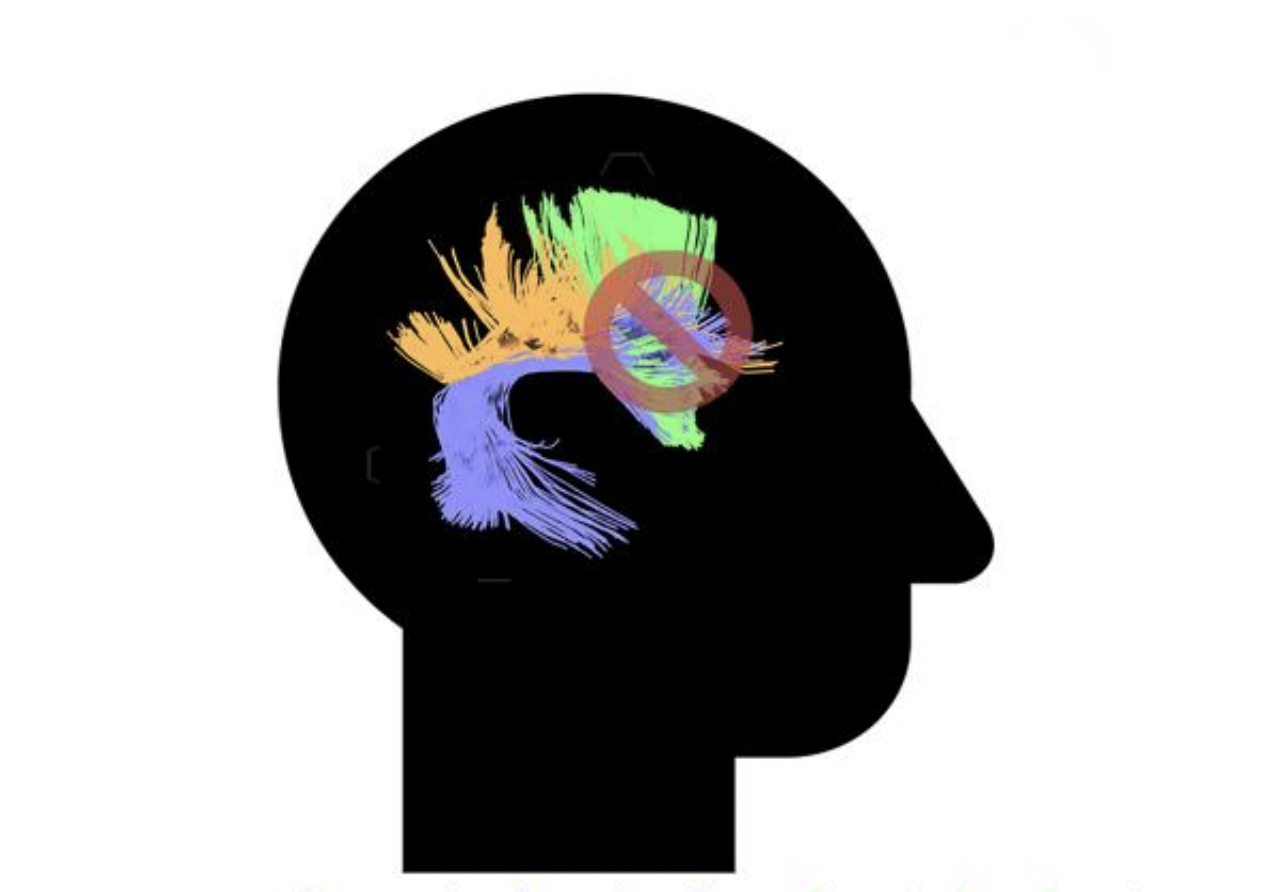
Successful communication depends on a multitude of factors, including the ability to produce information that is relevant for discourse between individuals in a real-world setting. This is one of the features of communication that can be disrupted in individuals with post-stroke aphasia, an acquired language impairment that can impact language production or comprehension.
Author: Sean Roberts
The Fall 2023 Edition of the MossRehab TBI Model System’s Brain E-News is Released
The researchers, clinicians, and staff at the MossRehab Traumatic Brain Injury (TBI) Model System have been busy and productive over the last several months and are excited to share news and updates in the latest edition of Brain E-News. This edition includes information about their recent presentations at the National Academy of Neuropsychology (NAN) Annual Meeting held in Philadelphia, PA, in October. The newsletter also shares new research examining the relationship between adverse experiences during childhood and health after brain injury, as well as updates on an ongoing collaborative research project focused on developing a program to train inpatient rehabilitation staff how to best communicate with patients after brain injury to maximize learning and performance during rehabilitation. In addition, there are staffing updates from the Elkins Park Empowerment Group, which provides support for people with TBI and their families and caregivers.
Dr. Rabinowitz Among Experts Involved in Updating Diagnostic Criteria For Mild Traumatic Brain Injury
Amanda Rabinowitz, PhD, Associate Director at MRRI, contributed as one of the collaborating authors in the recent publication of the updated diagnostic criteria for mild traumatic brain injury (TBI) by The American Congress of Rehabilitation Medicine (ACRM). This significant initiative, spearheaded by Noah Silverberg, PhD, Chair of ACRM’s Brain Injury Interdisciplinary Special Interest Group Mild TBI Taskforce, represents the first revision of ACRM’s widely utilized definition of mild TBI in three decades.
MRRI’s Brain Injury Neuropsychology Lab Welcomes Three New Research Assistants
MRRI is delighted to have a diverse staff of scientists, clinicians, trainees, and research support personnel. This month, the Brain Injury Neuropsychology Laboratory, directed by Amanda Rabinowitz, PhD, welcomed three new research assistants, McKenzie Buszkiewic, Dennis Tirri, and Julia Witkowski, who will work on a variety of projects in the lab.
Another Step Forward: NIH Designates People with Disabilities as a Population with Health Disparities
On September 26, 2023, the Director of the National Institute on Minority Health and Health Disparities (NIMHD), Eliseo J. Pérez-Stable, MD, announced that people with disabilities are now designated as a population with health disparities for all research supported by the National Institutes of Health (NIH). This designation will have far-reaching impacts in terms of increased representation and consideration in NIH-funded research, and ultimately, improved health outcomes for people with disabilities. We anticipate these impacts will be particularly pronounced for people with disabilities who also belong to other minority groups, a segment of the population which has faced tremendous inequities in healthcare and beyond.
MRRI Welcomes New Postdoctoral Fellow Dr. Jonathan Wood
This month, MRRI is excited to welcome a new postdoctoral fellow, Jonathan Wood, PhD. In his new role, Dr. Wood will be working with Aaron Wong, PhD, MRRI Institute Scientist and Director of the Cognitive-Motor Learning Laboratory.
Language Research Collaborations Between MRRI and University College London Continue to Grow
Aphasia, a communication disorder which affects how we understand and use language, affects millions of individuals worldwide, with around one in three people experiencing some degree of aphasia following a stroke. The impact of aphasia on quality of life can be devastating, and the need for innovative, evidence-based and effective therapies is growing. An ongoing collaboration between the laboratories of University College London Professor of Psychology and MRRI Scientist in Residence Gabriella Vigliocco, PhD, and MRRI Institute Scientist Laurel Buxbaum, PsyD, has been exploring how linguistic communication that is enhanced with gestures and other visual cues may benefit the language comprehension and production of people with aphasia (PWA). One ongoing project being run at both sites employs a unique paradigm with interactive card games to capture ‘real life’ communication of PWA. In August, UCL PhD student Isobel Chick, MSc, and Professor Vigliocco visited MRRI’s Cognition and Action Laboratory to discuss the latest updates from the study with Dr. Buxbaum and postdoctoral fellow Amy Lebkuecher, PhD.
MRRI Researchers are Presenting at the National Academy of Neuropsychology
The mission of the National Academy of Neuropsychology (NAN) is to advance neuropsychology as a science and health profession, to promote human welfare, and to generate and disseminate knowledge of brain-behavior relationships. NAN’s annual conference is being held in Philadelphia from October 25th-28th, providing the opportunity for MRRI researchers to attend and present research findings that are hot off the presses. Academic conferences provide an invaluable platform for scholars and researchers to present their work, receive constructive feedback, and refine their ideas, contributing to their professional growth. Conferences also provide a venue for emerging scholars to gain recognition in the field, leading to career advancement and new opportunities.
Former MRRI Postdoctoral Fellow Dr. Masahiro Yamada Begins New Faculty Position
Masahiro Yamada, PhD, began his postdoctoral fellowship at Moss Rehabilitation Research Institute (MRRI) in December 2020 under the guidance of his mentor, Shailesh Kantak, PT, PhD. At MRRI, Masahiro expanded his knowledge and expertise in neuroscience, utilizing transcranial magnetic stimulation (TMS) to elucidate motor control mechanisms of post-stroke patients.
MRRI Scientist in Residence Dr. Lyn Turkstra Visits the Institute
Scientific exchange and collaboration are often critical for developing and advancing world-class research programs. This was the motivation behind the development of MRRI’s Scientist in Residence program. Last month, MRRI was excited to welcome Lyn Turkstra, PhD, CCC-SLP, BC-NCD(A), for an in-person visit to the Institute. Dr. Turkstra is a Professor in the School of Rehabilitation Science at McMaster University, and she has been a Scientist in Residence at MRRI since 2019. During her visit, Dr. Turkstra connected with MRRI researchers including MRRI Associate Director, Amanda Rabinowitz, PhD, to work on collaborative research projects focused on cognition and communication after brain injury.