Successful communication depends on a multitude of factors, including the ability to produce information that is relevant for discourse between individuals in a real-world setting. This is one of the features of communication that can be disrupted in individuals with post-stroke aphasia, an acquired language impairment that can impact language production or comprehension.
At MRRI, Erica Middleton, PhD, Institute Scientist and Director of the Language and Learning Lab is an internationally recognized expert in aphasia research. “Both the ability to communicate relevant information during speech and the speed at which an individual is able to produce that information are key for successful communication,” remarked Dr. Middleton. “We know that impaired communication is linked to poorer health outcomes after stroke and lower quality of life. We need to develop rehabilitation approaches that can address the wide array of language impairments that people with aphasia experience,” she continued.
Developing effective, comprehensive, and personalized language rehabilitation therapies requires a better understanding of the neural substrates involved in different aspects of language and identifying biomarkers that can indicate which patients will likely benefit from which rehabilitation approaches.
Findings from a new research study published in the journal Brain Communications, shed light on the neural pathways that may be involved in producing discourse-relevant content in people with post-stroke aphasia. Neuroimaging measures of the integrity of these pathways may serve as useful biomarkers to identify people who have impairments in this aspect of communication and may benefit from targeted therapies.
In this study, Junhua Ding, PhD, his advisor at the University of Edinburgh Daniel Mirman, PhD, and Dr. Middleton examined data from eighty participants with chronic left hemisphere stroke that resulted in impaired language. They used correct information unit (CIU) analysis to quantify how informative each participant’s speech was during spoken discourse. Advanced neuroimaging methods (multivariate lesion-symptom mapping, voxel-wise disconnection, and tract-wise analyses) were then used to determine the relationships between speech impairments (CIU measures) and participants’ stroke lesions.
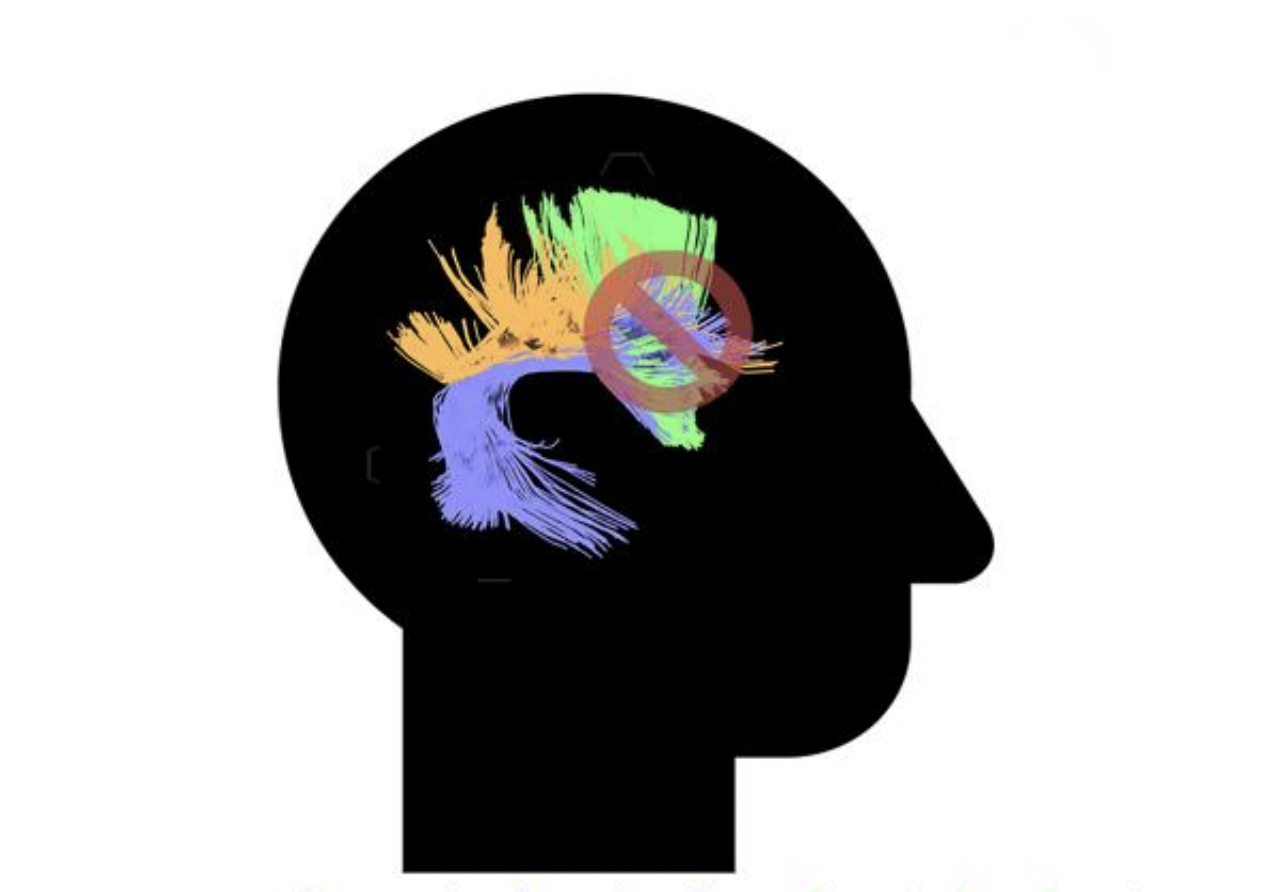
Their results showed that participants with more severe impairments in their ability to produce relevant information in discourse had greater damage to anterior dorsal white matter pathways in the brain, specifically the arcuate fasciculus, frontal aslant tract, and superior longitudinal fasciculus. These relationships were present both for the quantity and speed of informative speech production. They also discovered a strong association between total lesion size and deficits in spoken discourse production, where individuals with larger lesions tended to have greater communication impairments.
Results from this study are important because they have identified these anterior dorsal white matter pathways in the brain as critical structures for informative communication. The integrity of these pathways could be used as a potential biomarker for impairments in informative communication to identify patients for inclusion in clinical trials testing novel language rehabilitation strategies or to ultimately better personalize neurorehabilitation therapies in the clinic. “We are excited about these recent findings, as they represent an important piece of the puzzle we are putting together to better understand the neural underpinnings of language impairments. This is critical for developing the most effective rehabilitation approaches to maximize language recovery after stroke,” Dr. Middleton remarked.
Image above adapted from the manuscript graphical abstract: