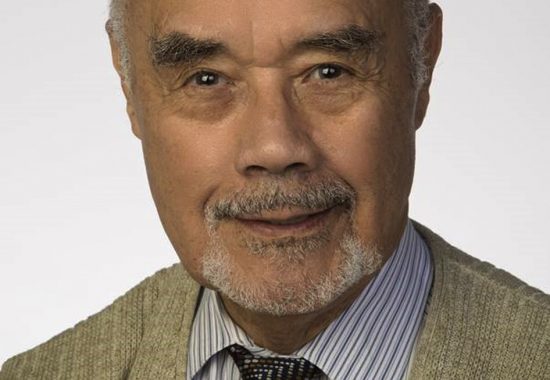
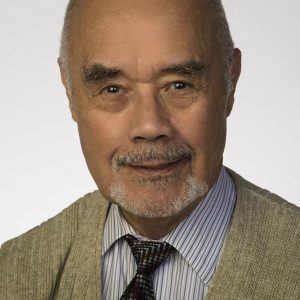
Finding the right mentor at the right time can have a tremendous impact on the trajectory of an early-career scientist. MRRI Institute Scientists are outstanding mentors who are invested in helping train the next generation of researchers in neuroscience and neurorehabilitation. Frank Garcea, PhD, was a postdoctoral fellow at MRRI from September 2017 through August 2020 under the mentorship of Laurel Buxbaum, PsyD, and he has been successful in establishing his independent research program at the University of Rochester Medical Center. In this interview, Dr. Garcea talks more about his experiences at MRRI and his current research.
Can you tell us more about your current position and what you are doing now?
After completing a three-year postdoctoral fellowship at MRRI in 2020, I moved to the University of Rochester Medical Center to begin a postdoctoral research position in the Neurosurgery Department. I then accepted a faculty position in the Neurosurgery and Neuroscience Departments in 2022. In my current position, I spearhead a cognitive neuroscience research lab composed of full-time research assistants, undergraduate students, master’s, MD, and PhD students.
What are your current research interests?
We use a range of neuroimaging and neuropsychological methods to study the structure and function of the human brain/mind. From a basic science perspective, our goal is to advance understanding of the cognitive systems supporting activities of daily life, like object manipulation and language production. Much of our work in this context uses functional MRI, diffusion tractography, and voxel-based lesion-symptom mapping to test hypotheses. One exciting problem we’re working on is to better understand how acquired brain injury to one area within a network can disrupt processing in areas outside the site of injury. This puzzling phenomenon is referred to as diaschisis, and its cognitive and neural bases have been investigated for over a century.
From a translational perspective, our goal is to use neuroimaging to support the planning of neurosurgical procedures here at the University of Rochester Medical Center. For example, if a patient has a brain tumor invading the motor cortex, my lab uses functional and structural MRI to identify where sensory, motor, and cognitive functions are represented in relation to the lesion. With this knowledge, our neurosurgery colleagues can tailor their surgical approach to avoid resecting cortical and subcortical tissues identified in our pre-operative mapping. As patients recover from their brain surgery, they are invited to take part in neuropsychological testing, which allows us to relate pre- and post-operative changes in cognitive function to the location of the lesion, the size of the neurosurgical resection, the type of brain pathology, etc.
What was it like working at MRRI and conducting research in MRRI’s Cognition and Action Lab?
Training at MRRI was a tremendous experience. I benefitted from a structured training plan, the regularly scheduled T32 lectures and workshops, and the opportunity to learn from experts in the cognitive and brain sciences. Working in Dr. Buxbaum’s lab was a fantastic experience on multiple levels. I was familiar with Dr. Buxbaum’s research interests, publications from her lab, and how research was conducted. Because of this, it was easy to embed my postdoctoral training within the broader goals of her lab, to collect neuroimaging and cognitive data, and to apply for extramural grants and publish manuscripts within a short time period.
Are there particular things you learned or skills you developed at MRRI that have helped you in your career?
I came to MRRI right after I finished my PhD. At the time, I understood that running a lab while competing for funding was a huge challenge. Because I had protected training time, I was able to learn how to write grants while also conducting research. I also learned that this is a skill that can take years to hone, so it was important to be patient and learn as much as possible while I had the protected time to do so. The experience was incredibly important for my career development, and I’m very appreciative of the faculty and staff at MRRI who took the time to review my grant proposals and provide critical feedback.
What were the next steps of your career after finishing your postdoctoral fellowship at MRRI?
This is the part of the story where my career development was affected by the COVID-19 pandemic. I finished my postdoctoral fellowship at MRRI in August of 2020. At that time, there were hiring freezes at universities across the country, which made finding another position challenging. I’m from Rochester, NY, and I did my PhD training at the University of Rochester. I moved back home in the spring of 2020 to be closer to family and was lucky to find a postdoctoral position in the Neurosurgery department here at the University of Rochester Medical Center (URMC). I then began writing grants immediately upon starting the position and was fortunate to secure a KL2 career development grant through the Clinical and Translational Science Institute here at URMC. This two-year fellowship provided vital resources to facilitate my career development and transition to a faculty position here at URMC.
Can you describe what it was like for you to launch your own independent research laboratory?
It’s rewarding and demanding all at once. With the KL2 funds, I was able to marshal resources and support to start building my lab. Hiring and training full-time research staff to coordinate day-to-day activities was a challenge because of COVID restrictions. Once I had staff trained and ready to go, my lab expanded in exciting ways. I was able to carve out some time to train undergraduate students and medical students working on projects. I’ve been fortunate to have kind and motivated students work in my lab. Probably the most rewarding aspect of running a lab is watching students develop their scientific skills and independence over time. Though it has been less than two years, I’m enjoying the environment, the culture of my lab, and the scientific content driving our projects forward.
What have been some of the biggest challenges you have had to overcome in your career or research?
Of the many challenges, I’d say the most challenging was recognizing and accepting my limitations. For years I’ve felt comfortable balancing the demands of multiple projects. Though it feels great to publish manuscripts and secure grant funding, this line of work can really wear one down without a proper work-life balance. As I started building my lab, I realized there are probably 5 – 10 tasks on my to-do list every day. I found that when I crossed a task off the list, a new task appeared. It’s overwhelming. I had to learn to say ‘no’ to new projects and to prioritize certain activities while putting other tasks on the back burner. This is incredibly difficult for me. Though I wouldn’t say I’ve ‘figured it out’, I do believe I’ve identified a strategy that allows me to stay productive while also maintaining my mental health.
Do you have a favorite scientific success story from your work?
It’s tough to pick just one! On a personal note, I’m thrilled that I’ve maintained a close relationship with my mentors. Earlier this year, I shared a meal with my postdoc advisor (Dr. Laurel Buxbaum) and my PhD advisor (Brad Mahon, PhD). We had a great time discussing problems we’re working on and challenges in our field. I feel truly blessed that I can call them up on the phone and ask for advice and know they’d be there to support me. I hope to be that person in the lives of the next generation of trainees whom I mentor.
On the scientific side, I’d say one success story that is front of mind is having students in my lab prepare manuscripts for publication. It’s incredible to see a person grow and develop when provided with the right resources and support. This is what success looks like from my point of view.
Knowing what you do now if you could go back in time and give advice to yourself when you were just starting your postdoc, what would you say?
I would tell myself to slow down and be patient. We often view success through the lens of papers published or grants funded. These endeavors can take years to accomplish. Life moves pretty fast, so appreciate the little victories and trust the process. I would also tell myself to go to more concerts! The music scene in Philadelphia is truly special. Though I had a great time seeing some of my favorite bands, I could have branched out and done more. I guess I would tell myself to be more present and enjoy living in Philadelphia while you have the opportunity.
How do you like to spend your free time?
Most of my family and friends live here in Rochester, so I’m lucky that I get to see them often. I’m also fortunate that I have a loving and supportive partner who enjoys traveling. We like to find new restaurants and places to visit in Rochester and in the Finger Lakes area. Upstate NY has a lot to offer in terms of history and culture, so we make a conscious effort to visit attractions close to us and outside of Rochester. In addition, I’m pretty regimented when it comes to working out and running. It helps to clear my head and is a huge stress reliever. I still try to go to concerts as often as I can. Last but not least, I enjoy spending time with my dog Rosie!