For more than a decade, researchers and clinicians in the field of rehabilitation have been searching for an answer to the black box problem—that is, the field’s inability so far to characterize and ultimately classify rehabilitation treatments according to useful, operational definitions that focus on their active ingredients.
In 2014, researchers at the Moss Rehabilitation Research Institute (MRRI), together with Marcel Dijkers, PhD and colleagues at the Icahn School of Medicine at Mount Sinai in New York, introduced an early framework for this process, called the Rehabilitation Treatment Taxonomy (RTT).
Since then, with support from the Patient-Centered Outcomes Research Institute (PCORI), this project has progressed and transformed into the Rehabilitation Treatment Specification System (RTSS). Four upcoming (2018) publications will outline advancements that have taken place during the most recent grant cycle.
“Our earlier work on this project, led by Marcel Dijkers, under a National Institute on Disability and Rehabilitation Research (NIDRR) grant, allowed us to flesh out the concepts underlying our attempts to define treatments with respect to their active ingredients,” says John Whyte, MD, PhD, founding director of MRRI. “However, we didn’t get to the point of crafting actual procedures, or how-to steps for specifying treatments according to those concepts. During this cycle, the goal was really to move the project to that level—to apply the concepts we had developed in a procedural way, to help guide clinicians and researchers in more clearly defining their rehabilitation treatments.”
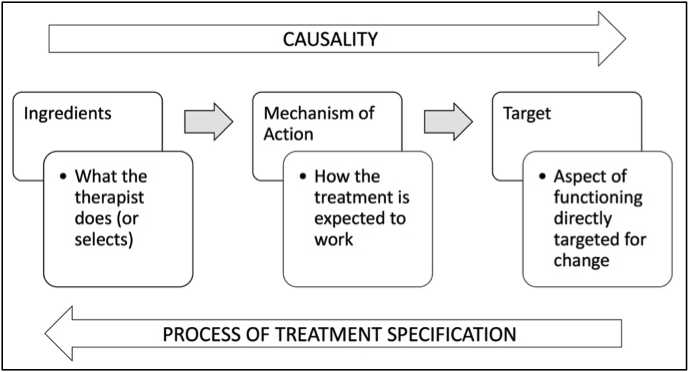
The tripartite structure of treatment theory. Ingredients launch a mechanism of action that acts to change the functional target of treatment. The clinician’s reasoning process works in reverse: beginning with a treatment target that requires change, the clinician considers mechanisms that could change it, and selects the ingredients to produce those mechanisms.
A procedural manual that offers users a step-by-step process for specifying rehabilitation treatments is now ready for beta testing. The American Congress of Rehabilitation Medicine (ACRM), an early champion and advocate of this project, is currently exploring the feasibility of hosting the manual on their website. An immediate goal is to have clinicians begin to use the manual with an application that allows the site to collect feedback. You can gain access to the manual here.
“After distilling feedback from our excellent advisory board, the clinicians we have trained, and others who have attended our presentations, we learned that our concepts are indeed valuable, and could make an important difference in the field,” says Dr. Whyte. “However, they are complex, and a manual alone can’t make them simple. We learned that people need frequent and continuous exposure to these concepts—that using these concepts is itself a skill that requires practice and feedback.”
Some project highlights
Earlier work on the RTT, toward developing a system for classifying rehabilitation treatments and services based on their active ingredients, proceeded with the goal of facilitating the study and dissemination of treatments, enabling clear communication about them, and improving clinician training. However, as work on the RTT progressed, the need for an interim stage of the project emerged.
“Since the active ingredients of a treatment ultimately determine whether it is effective, we wanted to build a taxonomy based on the active ingredients of various treatments,” says Dr. Whyte. “However, while working on this project we realized that we must be able to specify treatments based on their active ingredients first, before we can create a taxonomy built on those active ingredients. The process of specifying treatments does not automatically result in a taxonomy—for example, developing a list of 1,000 well-described treatments is not the same as sorting them into categories. We began to recognize treatment specification and treatment categorization as two different steps in our ongoing effort. In other words, an RTSS must precede an RTT.”
The RTSS has retained and furthered the development of many of the project’s earlier concepts. The concept of volitional treatment, for example, underwent significant elaboration during work on the RTSS.
“This has been one of the significant obstacles we’ve faced in our attempts to describe and define treatments,” says Dr. Whyte. “Many, if not most, rehabilitation treatments involve some type of active involvement on the part of patient, and because it’s not possible to anticipate exactly what a patient will do during such an interaction, it is difficult to fully define a volitional treatment in advance.”
The problem of volition is not unique to rehabilitation, notes Dr. Whyte. Although a drug may exert an effect on a passive patient, for example, the patient must take the drug for it to have an effect. Similarly, a clinician may design an activity for a patient to practice repeatedly, but the patient must practice.
“In the RTT we already had made an important distinction between a volitional treatment—any treatment that requires the patient to exert effort—and passive treatments. But we had not yet created rules for defining volitional treatments that clarified both the functional target and the “volition target,” with the functional target being, for example, increased strength in certain muscles, and the volition target being that the patient lift weights in the right way a certain number of times.”
The procedural rules of the RTSS distinguish between treatments delivered in person, during face-to-face encounters, and those that take place at home or in environments where a clinician is unable to supervise a patient’s performance. For face-to-face encounters, functional and performance targets are combined, with the understanding that in these encounters a clinician can adjust the ingredients in real time to ensure performance of the exercises. The RTSS specifies these targets separately when a patient is instructed to engage in an activity at home, or when a clinician is not present, since the instructional and motivational ingredients must be carefully planned in advance.
“We had to make difficult decisions when it came to determining how volitional treatments should be specified. We found that there was not a perfect formula for doing this, so we ended up with a tradeoff between precision and utility. But the RTSS emphasizes the importance of acknowledging that these two phenomena play separate roles in efficacy, particularly when training clinicians in the administration of volitional treatments or when engaging in comparative effectiveness research.”
Encouraging familiarity with RTSS concepts
The RTSS should eventually enable researchers to use a common framework for systematically testing the effects of specific ingredients on specific targets, and in turn for more readily replicating them and translating them into clinical practice. Toward that end, the forthcoming 2018 publications extend an invitation to researchers and clinicians who may want to implement the RTSS in local projects and help develop the concepts further. To pave the way for adoption of the RTSS, it will be essential to encourage clinical education programs to take up these concepts in their curricula, convince grant reviewers to make use of these concepts when reviewing treatment grants, and inspire journal publishers and reviewers to take up these concepts when reviewing articles for publication.
“This project has already spawned smaller projects here at Moss,” says Dr. Whyte. “For example, one project involves training clinicians in these concepts with the goal of improving the clarity of coverage notes. The goal is to help therapists communicate a treatment or exercise—let’s say gait training—in a way that more clearly specifies clinician behaviors and other elements of a treatment, and that will allow a covering therapist to deliver consistent care.”
Other projects are evaluating whether specifying treatments in the RTSS format in various publications is helpful for authors and readers. And trainees in MRRI’s postdoctoral neurorehabilitation research training program are also exposed to these concepts.
“In addition to inspiring future projects,” says Dr. Whyte, “we hope, of course, that these concepts will inform the way that post docs do their research here at MRRI.”


1,598 comment on “Developing a Rehab Treatment Specification System”