This week, Moss Rehabilitation Research Institute (MRRI) welcomes postdoctoral researcher Amy Lebkuecher, PhD. Dr. Lebkuecher will be furthering her scientific training under the joint mentorship of Laurel Buxbaum, PsyD, Associate Director of MRRI, as well as H. Branch Coslett, MD, Professor of Neurology at the Perelman School of Medicine at The University of Pennsylvania.
Dr. Lebkuecher completed her undergraduate training in psychology at East Stroudsburg University. She then enrolled in a graduate program at Lehigh University where she was awarded a Masters of Science degree in psychology. Afterwards, Dr. Lebkuecher worked as a study coordinator at Kessler Foundation. In this position, she contributed to research on cognitive rehabilitation in individuals with multiple sclerosis and traumatic brain injury. Dr. Lebkuecher was recently awarded her PhD in Psychology and Language Science from The Pennsylvania State University.
Her graduate research investigated commonalities between language (linguistic) and nonlinguistic domains of cognition, particularly motor planning. A focus of her recent work has examined parallels in planning biases and error patterns across motor planning and language. In another line of research, she has investigated the connection between language and other nonlinguistic domains of cognition, such as learning and attention, in individuals with and without a history of language disorder. Findings from her dissertation research demonstrate that individuals with a history of language disorder do not attend to regularities in the environment in the same manner as individuals without a history of disorder. This difference could contribute to the variable language outcomes observed across these populations. Dr. Lebkuecher has received multiple awards for her early career research, including the Research and Graduate Studies Office Dissertation Award and the Donald A. Trumbo Research Award, both from The Pennsylvania State University.
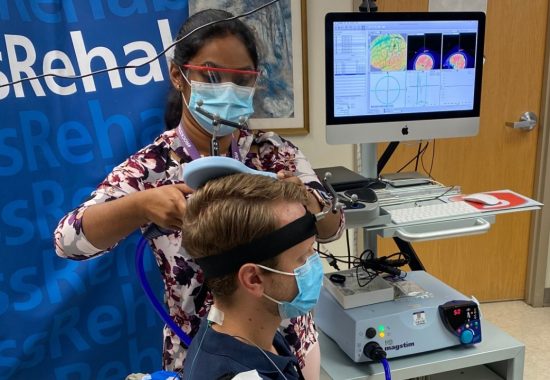
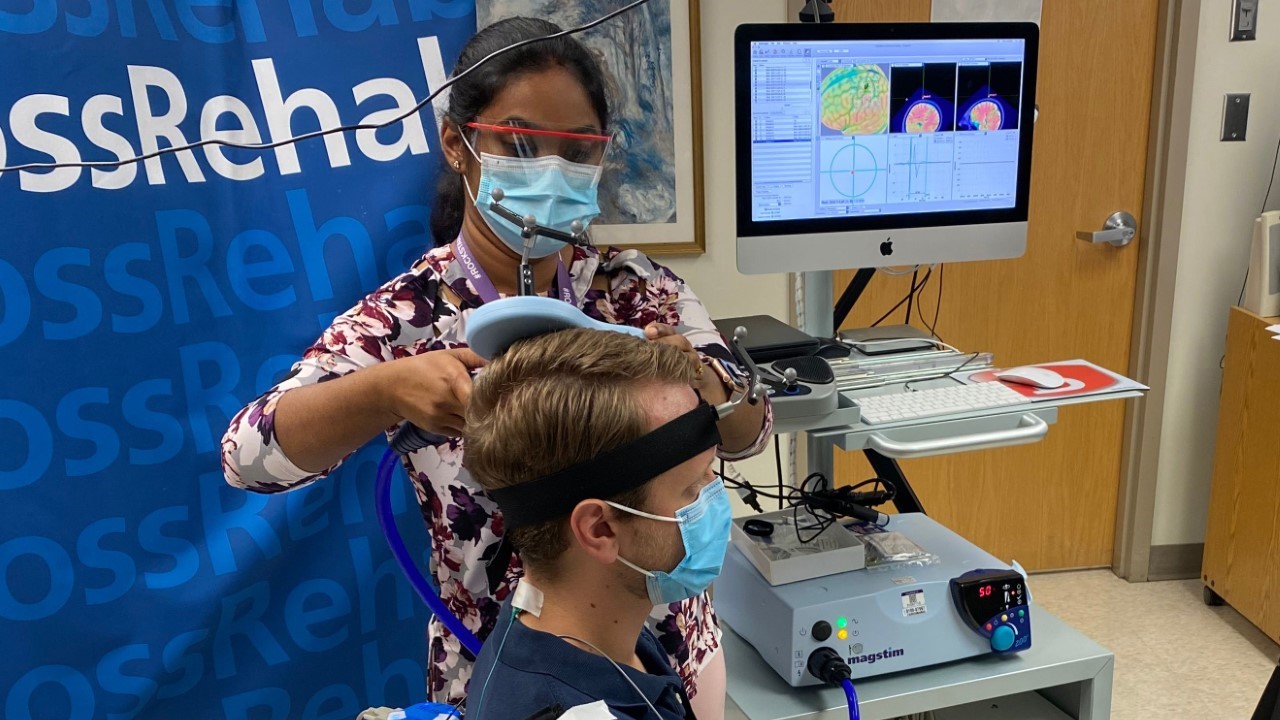
At MRRI, Dr. Lebkuecher will continue to investigate the connection between language and motor domains by evaluating motor and language abilities in patients with aphasia or apraxia resulting from left-hemisphere stroke. Aphasia is an acquired language disorder that affects a person’s ability to express and understand language. Apraxia is a movement disorder where individuals have difficulty performing skilled movements. Dr. Lebkuecher also looks forward to continuing her research on analogous error patterns across motor planning and language domains. In this work, she will examine electroencephalography (EEG) signals to determine whether they reflect error detection in individuals with aphasia or apraxia caused by left-hemisphere stroke, as well as in neurotypical individuals.
In the long term, Dr. Lebkuecher hopes to develop a research program that will elucidate the connection between language, motor planning, and other non-linguistic domains of cognition to improve our basic understanding of human cognition, as well as to inform rehabilitation treatments for individuals with various motor and cognitive deficits.