The World Health Organization estimates that 250,000 – 500,000 people globally experience a spinal cord injury each year, and these injuries often lead to substantial long-term disability, impacts on quality of life, and high economic costs. Despite substantial investigation in this area of research, scientists have not yet identified a way to trigger damaged neurons in the human adult spinal cord to successfully regenerate or regrow.
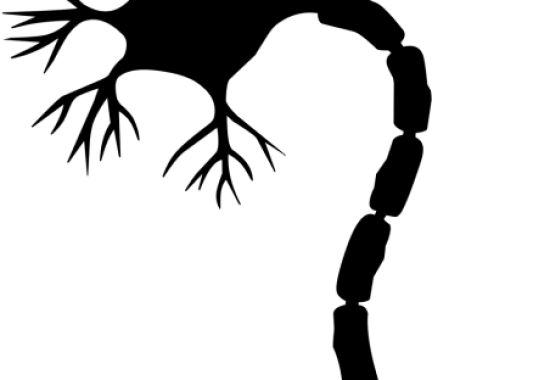
In particular, researchers have been investigating various signaling pathways that are active during early development when these axons naturally grow, as well as the physiological changes that occur afterward that prevent neuronal regrowth and regeneration once development is completed. During development of the central and peripheral nervous system, long-distance axon growth is mediated in part by a biochemical pathway within neurons called the RAF–MAP2K (mitogen-activated protein kinase kinase) signaling cascade. This pathway has been identified as a potential target for intervention to facilitate axon regrowth and regeneration after spinal cord injury.
In order to evaluate new potential treatments for spinal cord injury, a critical step is examining the impacts of these interventions in animal models. Further research can then focus on translating these results to develop treatments appropriate for clinical application in humans.
In work led by researchers at Burke Neurological Institute and Weill Cornell Medicine, researchers investigated whether the RAF–MAP2K signaling cascade could be activated using genetic engineering and noninvasive stimulation to promote axon sprouting and functional recovery in the adult nervous system in mice. Their recent findings represent a significant advancement in the translation of a potential non-invasive treatment approach to promote motor recovery after spinal cord injury.
Dylan Edwards, PhD, MRRI Director and Director of the Human Motor Recover Laboratory, is a co-author on the paper recently published in Science Translational Medicine that details their experiments and findings. In particular, Dr. Edwards was instrumental in providing insight for the noninvasive stimulation protocols used in this research. Non-invasive stimulation methods such as repetitive transcranial magnetic stimulation (rTMS) show promise for enhancing recovery after nervous system injury, but there are still many unanswered questions regarding the mechanisms by which these methods confer benefits, the extent of recovery which may be possible, and the optimal parameters of delivery.
Using genetic approaches, the authors demonstrated that activation of BRAF (a protein kinase that plays a key role in the RAF–MAP2K signaling cascade) resulted in upregulation of transcription factors that were shown to be associated with neuronal development and neuronal regeneration in prior studies. Activation of BRAF was also associated with downregulation of transcription factors previously demonstrated to limit the capacity of axons to regenerate. In their subsequent experiments, the authors of this paper showed compelling evidence that BRAF activation allowed axon sprouting, formation of new synapses, and functional recovery in mouse models of spinal cord injury. These results suggest that conditions conducive to regeneration and regrowth can be induced in mature neurons in the corticospinal neurons via the RAF–MAP2K signaling cascade by activating BRAF.
Further, scientists determined that daily high-frequency rTMS sessions activated the RAF–MAP2K signaling pathway and also modulated the expression of the same set of transcription factors associated with regeneration. In addition, high-frequency rTMS resulted in axon sprouting, regeneration, and functional recovery in spinal cord neurons after injury. Moreover, researchers confirmed that a functional RAF–MAP2K signaling pathway was essential to achieving these results.
These findings are important because many genetic approaches used in animal models are not feasible for use in clinical applications in humans. High-frequency rTMS is a non-invasive method that has been demonstrated to be safe to use in numerous clinical research studies, and the results of this study strongly support that it may be an effective approach to facilitate regeneration and recovery after spinal cord injury.
Dr. Edwards and his colleagues have begun clinical trials of a high-frequency rTMS protocol in humans, and they will also continue to investigate related questions in animal models. This line of research has the potential to lead to the development of a non-invasive, low-risk treatment method for spinal cord injury and other nervous system injuries that could improve the lives of millions of people around the world.
This research was made possible by funding from the National Institutes of Health, the New York State Department of Health Spinal Cord Injury Research Board, the Craig H. Neilsen Foundation, the Wings for Life Research Foundation, the Goldsmith Research Foundation, and the Burke Foundation. You can read the published version of the original research article in Science Translational Medicine, and a full-text pre-print of the manuscript is also available on bioRxiv.


2 comment on “New Studies Advance Translational Neuroscience Research for Spinal Cord Injury”